From anecdotes to artificial intelligence tools, the way doctors make medical decisions is evolving with technology
Over the past 50 years, the practice of medicine has undergone an incredible but incomplete transformation, steadily evolving from a field that relied primarily on expert opinion and the anecdotal experience of individual clinicians to a formal scientific discipline.
The emergence of evidence-based medicine means that clinicians can determine the most effective treatment options for patients based on quality assessments of the latest research. Precision medicine now enables healthcare providers to leverage patients’ personal genetic, environmental and clinical information to further personalize their care.
The potential benefits of precision medicine also come with new challenges. Importantly, the amount and complexity of data available for each patient is increasing rapidly. How do clinicians determine which data are useful for a specific patient? What is the most efficient way to interpret the data to select the best treatment?
These are exactly the challenges that computer scientists like me are trying to solve. My colleagues and I work with experts in genetics, medicine, and environmental science to develop computer-based systems, often using artificial intelligence, to help clinicians integrate diverse and complex patient data to make optimal care decisions.
The rise of evidence-based medicine
As recently as the 1970s, clinical decisions were largely based on expert opinion, anecdotal experience, and theories of disease mechanisms, which were often not supported by empirical research. Around that time, some pioneering researchers argued that clinical decisions should be based on the best available evidence. By the 1990s, the term “evidence-based medicine” was introduced to describe the discipline that combines research with clinical expertise when making patient care decisions.
The cornerstone of evidence-based medicine is the hierarchy of evidence quality, which determines which types of information clinicians should rely most on when making treatment decisions.
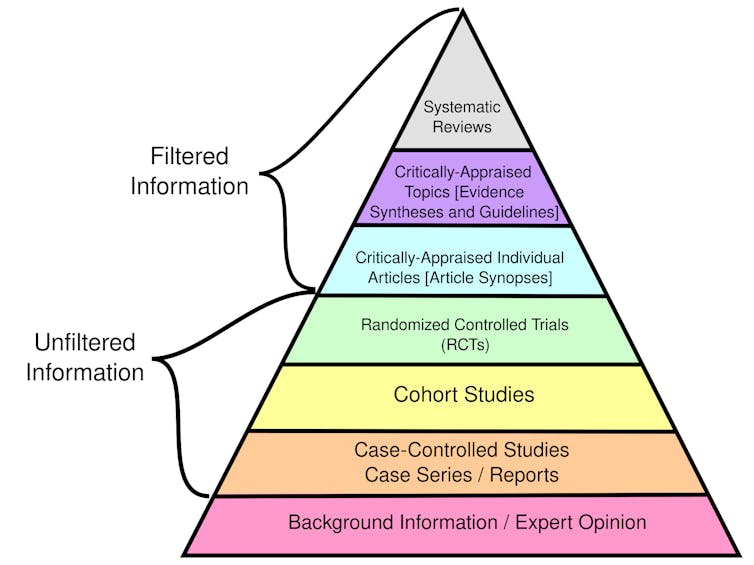
CFCF/Wikimedia Commons, CC BY-SA
Randomized controlled trials randomly divide participants into different groups to receive an experimental treatment or a placebo. These studies, also called clinical trials, are considered the best source of individual evidence because they allow researchers to compare treatment effects by ensuring the groups are similar with minimal bias.
Observational studies, such as cohort studies and case-control studies, focus on the health outcomes of a group of participants without any intervention from the researcher. Although used in evidence-based medicine, these studies are considered weaker than clinical trials because they do not control for potential confounders and bias.
Overall, systematic reviews that synthesize findings from multiple studies provide the highest quality evidence. In contrast, evidence from single-case reports detailing individual experiences is weak because they may not apply to the broader population. Likewise, personal evaluations and expert opinions are not themselves supported by empirical data.
In practice, clinicians can use an evidence-based medicine framework to formulate specific clinical questions about their patients that can be clearly answered by reviewing the best available research. For example, a clinician might ask whether statins are more effective than diet and exercise in lowering LDL cholesterol in a 50-year-old man with no other risk factors. Combining evidence, patient preferences and their own expertise, they can develop a diagnosis and treatment plan.
As expected, collecting and putting all the evidence together can be a laborious process. As a result, clinicians and patients often rely on clinical guidelines developed by third parties such as the American Medical Association, the National Institutes of Health, and the World Health Organization. These guidelines provide recommendations and standards of care based on a systematic and thorough evaluation of existing research.
The dawn of precision medicine
Around the same time that evidence-based medicine was gaining traction, two other transformative developments in science and health care were underway. These advances will lead to the emergence of precision medicine, which uses patient-specific information to tailor health care decisions to each individual.
The first was the Human Genome Project, which was officially launched in 1990 and completed in 2003. It attempts to create a reference map of human DNA, or the genetic information that cells use to function and survive.
This map of the human genome allows scientists to discover genes associated with thousands of rare diseases, understand why people respond differently to the same drugs, and identify tumor mutations that can be targeted with specific treatments. Clinicians are increasingly analyzing patients' DNA to identify genetic variations that could inform their treatment.
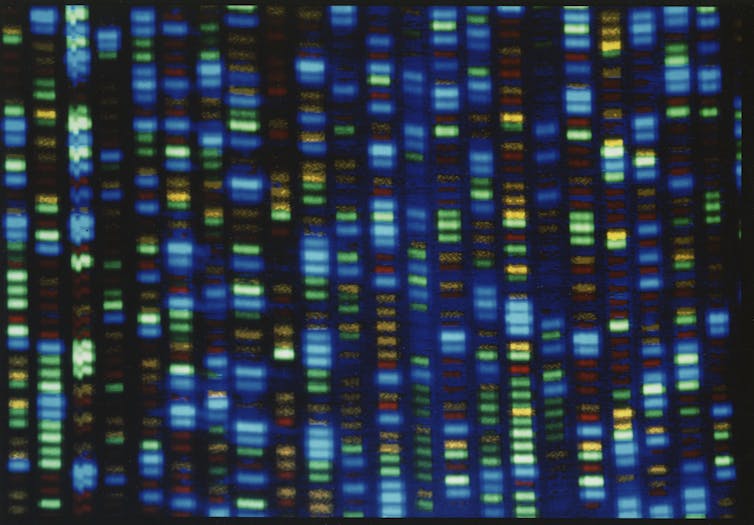
National Human Genome Research Institute/Flickr
The second is the development of electronic medical records to store patient medical history. Although researchers have been conducting pilot studies of digital records for years, the development of industry standards for electronic medical records did not begin until the late 1980s. It was not until the American Recovery and Reinvestment Act of 2009 that this technology became widely adopted.
Electronic medical records allow scientists to conduct large-scale studies of associations between genetic variants and observable characteristics, thereby informing precision medicine. By storing the data in an organized digital format, researchers can also use these patient records to train artificial intelligence models for use in medical practices.
More data, more artificial intelligence, more precision
On the surface, the idea of using patient health information to personalize care is not new. For example, the Framingham Heart Study, conducted since 1948, produced a mathematical model that estimated a patient's coronary artery disease risk based on their individual health information rather than average population risk.
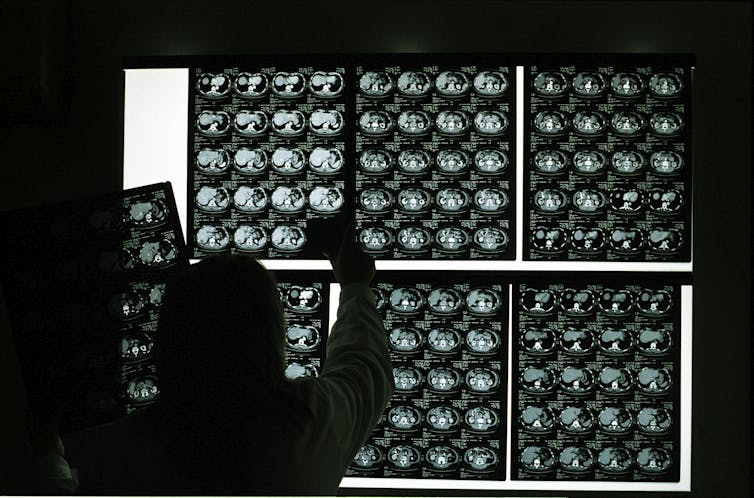
However, a fundamental difference between personalized medicine and electronic medical records now and before the Human Genome Project is that the mental capabilities required to analyze the scale and complexity of individual patient data available today far exceed the capabilities of the human brain. Each individual has hundreds of genetic variants, hundreds to thousands of environmental exposures, and a clinical history that may include numerous physiological measurements, laboratory values, and imaging results. In my team's ongoing work, the artificial intelligence model we are developing to detect sepsis in infants uses dozens of input variables, many of which are updated hourly.
Marco Vacca/Photographer’s Choice RF via Getty Images
Researchers like me are using artificial intelligence to develop tools that help clinicians analyze all this data to tailor diagnosis and treatment plans for each individual. For example, certain genes can affect how certain drugs work in different patients. While genetic testing can reveal some of these characteristics, screening every patient is not yet feasible due to cost. Instead, an AI system could analyze a patient's medical history to predict whether genetic testing would be beneficial based on the patient's likelihood of taking medications known to be affected by genetic factors.
Another example is diagnosing rare diseases, or conditions that affect fewer than 200,000 people in the United States. Diagnosis is difficult because many of the thousands of known rare diseases have overlapping symptoms, and the same disease can appear differently in different people. Artificial intelligence tools can help determine which characteristics may contribute to disease by examining a patient's unique genetic and clinical characteristics. These AI systems may include components that predict whether a patient's specific genetic variation negatively affects protein function and whether a patient's symptoms resemble those of a specific rare disease.
The future of clinical decision-making
New technologies will soon enable routine measurement of other types of biomolecular data beyond genetics. Wearable health devices can continuously monitor heart rate, blood pressure and other physiological characteristics, generating data that artificial intelligence tools can use to diagnose disease and personalize treatment.
Related research has yielded promising results in precision oncology and personalized preventive health. For example, researchers are developing wearable ultrasound scanners to detect breast cancer, and engineers are developing skin-like sensors to detect changes in tumor size.
Research will continue to expand our understanding of genetics, the impact of environmental exposures on health, and how artificial intelligence works. These developments will significantly change the way clinicians make decisions and provide care over the next 50 years.